Book: Emotional Well-Being for the Person with Dementia
| Сайт: | Dementia Family Carer E-Learning Courses |
| Курса: | Later Stage Dementia Care - Blended Learning for Families (Final Template) |
| Кніга: | Book: Emotional Well-Being for the Person with Dementia |
| Надрукавана: | விருந்தினர் |
| Дата: | нядзеля, 8 чэрвеня 2025, 11:57 AM |
1. Learning Goals
The objectives of this unit are to:
have an awareness of the importance of promoting emotional well being for the person with dementia
understand the principles of person-centred care
outline how you can provide emotional support at the end of life stage.
2. Introduction
This week explores the psychosocial needs of people with later stage dementia. By “psychosocial” we mean mental and social conditions that are important to health and wellbeing. Social conditions include relationships and home environments, while psychological conditions indicate the person's way of dealing with relationships and conditions, cognitively and emotionally.
This unit also explores the emotional wellbeing and dignity of the person with dementia. We will identify the universal needs of people at end of life, and consider those needs in the context of dementia.
You will also identify barriers to enhancing dignity and emotional wellbeing, and we will set out strategies to minimise those barriers. We will also look at interventions that can enhance emotional wellbeing. We will consider the importance of stimulation of senses.
Finally, we will examine the dying phase and consider how a person's needs change as they enter the last days of life.
3. Dignity and Human Rights
We at ASI advocate for and encourage a human rights approach to social relations and indeed to dementia care. Take a look at the words above that spell out a human rights for all approach.
The short video produced by The Alzheimer Society of Ireland highlights the needs and wishes of people with dementia, from a human rights standpoint.
In memory of Brian Doyle RIP 2020.
4. People's universal needs (Maslow's hierarchy)
All humans have fundamental and universal needs throughout life.
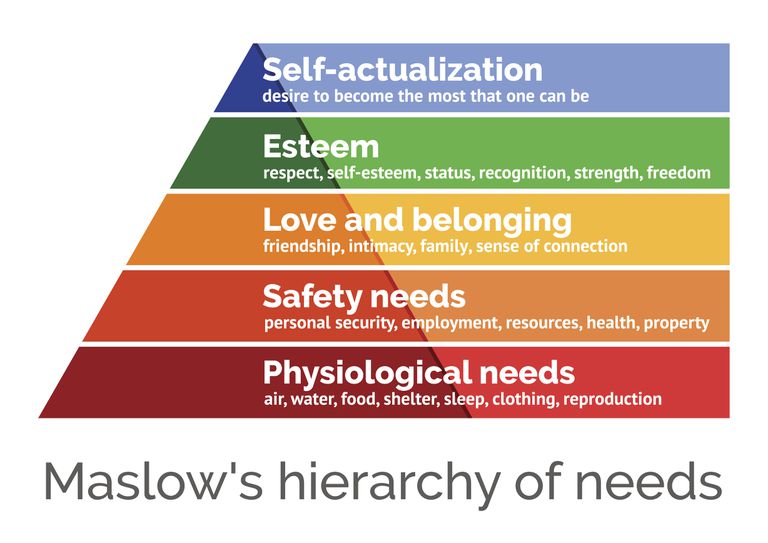
Maslow was an American psychologist who developed a theory of psychological health based on the premise that humans have an innate range of needs. Maslow described human needs as ordered in a predestined hierarchy—a pressing need would need to be satisfied before someone would give their attention to the next highest need.
The diagram is a visual representation of his work. It suggests that if a person’s Physiological Needs (the base of the pyramid) are met i.e. need for food, shelter, water, reproduction etc. then people are able to move on to the next ‘layer’ which is Safety. Safety Needs include the need for personal safety, need for a job etc. When these needs are met, a person may move on to next layer. It may take a life time to reach the top layer which is Self-Actualisation and some people may not reach it.
Many people can identify with Maslow’s hierarchy too. Carers need to have a sense of stability and security, feeling that they are in control of their own lives, having control over what is happening around them. This can be hard when caring for someone with dementia. Studies have shown that unmet needs for relational fulfillment in both partners may add to carers’ sense of burden.
People who have dementia may move down the pyramid as they lose memory of their life experiences. Even though they are declining, they are still adults with memories, experiences, and skills that have been acquired during their life. They still have needs.
5. Personhood in Dementia
All humans have fundamental and universal needs throughout their life perhaps most significantly during times of crisis and vulnerability. Many researchers have looked at ‘peoples needs’ in the context of dementia.
Professor Tom Kitwood (1997) emphasised the importance of a person’s with dementia needs and promoted person-centred dementia care. He said that considering people with dementia in purely medical terms takes away their identity. People are more than an illness; they are living a life, a life that has a story, a life within relationships. Kitwood called this ‘the recognition of personhood’.
We saw that Maslow was an original thinker and identified his Hierarchy of Needs for all people. Kitwood, specifically focussed on the person with dementia, identified six psychological needs. He didn’t propose them as a hierarchy but rather as a circle or a continuum.
We will look at these needs in the context of End of Life Care using a Palliative Care approach with a person centred care framework (terms discussed earlier in the course in Book: Introduction).5.1. Comfort
Comfort is one of the six psychological needs identified by Kitwood. It is perhaps the main concern at end of life.
It is defined as a state of physical ease and freedom from pain or constraints.
Maintaining physical and emotional comfort forms the mainstay of the palliative care approach to care - alleviating suffering rather than attempting to prolong life.
Comfort care also includes 'being with rather than doing for’. Try to set the kind of environment that most acknowledges the person's personhood. What has he or she always enjoyed?
So in the context of a long-term care environment, 'comfort' may mean different things to different people. For example, if Bill loved a party, it might be natural for him to want to be surrounded by family and friends. Perhaps Ellen always preferred spending quiet moments with one or two people at a time. It follows that she may be most comfortable with just a few visitors.
5.2. Love and Spirituality
Love is an elusive term that conjures up feelings and emotions of attachment and connection, of friendship and kindship and caring
Spirituality is also an elusive term that may or may not include religious needs. For some people it’s an important factor. Death is a profoundly significant event for all humans regardless of religious or spiritual beliefs. There has been research on the importance of spiritual support at end of life. People with dementia typically receive significantly fewer spiritual interventions than people without cognitive impairment.
In dementia and Later Stage dementia, love can be expressed through a sense of connectedness. Love and spiritual awareness can:
o Promote one’s identity
o Bring a sense of belonging and security
o Support the need for space and privacy and therefore enhance dignity
o Encourage people with dementia to participate in activities as much as is possible
o Celebrate special occasions and making every day special
o Bring strength in times of distress
o Help to maintain faith practice and contact with faith groups
And for Carers
o Welcome and affirm the contribution which people with dementia can make to the spiritual life of others
5.3. Identity
Research shows that for most of us ‘end of life’ includes being treated as an individual, with dignity, respect, without pain, in familiar surroundings in the comfort of close family and friends (Middleton-Green et al (2017).
Identity, can be conceptualised as a person’s life story. Life stories can be told through words, pictures or music. The time taken to construct a life story with the person you are caring for should enhance relationships, provide comfort, embrace love and provide dignity.
The telling of the person’s life story also presents a way for approaching support at end‐of‐life as it recognises that it is the final chapter of a life story. Attention to issues of identity and relationships is beneficial for the person dying and their carers. (Leonard, Horsfall et al, 2017)
Particularly, in the last year of life, people with dementia become vulnerable following a gradual and prolonged decline in abilities. If the person with dementia is being cared for in a familiar environment, by carers with whom they have a relationship, the maintenance of personhood is less challenging than if they find themselves in a busy hospital or unfamiliar environment where the carers may know little more than their name and diagnosis.
5.4. Attachment
An American psychologist Bowlby (1979) defined attachment as a 'lasting psychological connectedness between human beings'. Kitwood agreed and said that persons living with dementia should be part of relationships that treat them with dignity and respect, and where their individuality is always supported. This type of caring relationship is about being present and concentrates on the interaction, rather than the task. It is about “doing with” rather than “doing for”.
Due to the dementia disease, persons with dementia are dependent on others. The further the dementia advances, the greater the need for “person-work.” Carers need to be the support that maintains the person with dementia. Knowing the person is central to care that is based in mutual, trusting and caring relationship, Fazio (2017). Providing an environment that allows continuous relationships helps the person with dementia to feel secure and to feel attached.
5.5. Occupation and Inclusion
People at end of life have identified that the maintenance of normality
is important to them (Black 2011), though none of the research was dementia
specific.
The need for normality is doubtless present for people with dementia, even though the shape and presentation of that normality may have altered over the years, (Middleton-Green, 2017)
The importance of personhood remains vital to care given at this stage of life. The business man may feel the need to see or feel his brief case, the hairdresser may like seeing and touching a collection of brushes on the table, a mother may feel more comfortable being in the kitchen, surrounded by activity.
Being valued for who we are and have been is important. It facilitates identity, brings comfort and supports dignity.
6. Unit 4 Case Study
Maura has put in an ‘office’ for Tony to do ‘paperwork’ and bought some indoor plants for him. This worked well for a number of months and Tony got great enjoyment/distraction from it. However lately he is becoming more agitated and frustrated and the ‘office’ or plants don't seem to be helping.
Yesterday, when Tony was outside in the garden, he used a golf club to break the kitchen window.
Maura has decided to contact the GP/Psychiatry of Later Life. She is waiting for a home visit this week.
1. What do you think Tony might be feeling? Can you offer any possible reasons for Tony’s behaviour?
2. What non-medical interventions could help Maura and Tony in this situation?
3. What questions should she ask the Psychiatry of Older Age team? What treatments do you think they could offer?
4. How do you feel about medications for this situation?
Please post up your thoughts and answers to these questions on the Forum: Unit 4 Discussion. Thank you.7. End of life - connecting with the person
The Later Stage of Dementia is a time to transcend traditional modes of care and create a compassionate environment in which somebody can experience a peaceful end of life and death.
People with dementia may be unable to communicate their needs directly but the physical senses remain. People with dementia can feel, touch, smell scents, and hear sounds albeit in an altered or diminished capacity. It is possible to create a meaningful environment that respects the person within. This time allows for the creation of opportunities for connection and compassionate care using the senses. Let's look at some of these senses now.
7.1. Touch
From the beginning of our life, through to the end of life, humans respond to tactile stimulation, though touch can bring different meanings to different people. Non-medical researcher Guerrero (2017) reports that touch is the best way to comfort. In nonverbal and emotional communication, touch is particularly noteworthy; "We feel more connected to someone if they touch us."
In palliative care, comfort measures assume greater significance. Touch is a powerful way of facilitating communication. It can enhance psychological and physical comfort. It denotes presence. It denotes human connectedness (Sims 1988)
As care needs progress, somebody with dementia may only experience touch in the context of being washed or changed, or undergoing medical interventions. The simple act of physical contact—holding hands, a touch, or a gentle massage—can make a person feel connected to those he or she loves. It can be very soothing.
In considering the person (person centred care) we must remember that some of us aren’t comfortable with touch.
7.2. Scent
Some odours evoke memories....
Did the person with dementia work in a bakery? In a hairdressers? Live near a farm or a brewery?
Scents may be potential avenues of communication and connection. Aromatherapy is increasingly used in dementia care, for example lavender oil significantly reduces aggression in elderly patients with dementia (Michaelson, Knight and Fink, 2002)
7.3. Sound
The brain's auditory system remains intact and responsive to music and sounds long after other parts of neurological functioning have ceased (Robinson, 2001).
The Live Inside video below shows the benefits of music therapy for the person with late stage dementia. Please click the play button to watch the video:
7.4. Sight
Ageing can bring changes in a person’s eyesight including the presence of cataracts, glaucoma and/or macular degeneration. As dementia progresses, there are numerous changes associated with eyesight.
Some people with dementia have difficulties perceiving in three dimensions, some need brighter lighting, some may have reduced contrast between colours and some reduced peripheral vision.
When creating a calm, comforting space for those at end of life, sensitivities to light and sight need to be considered. Avoid placing objects in peripheral vision only. Quality and intensity of light is important. Light is known to affect the quality and quantity of sleep. An awareness that some people with dementia have hallucinations and delusions may be helpful.
8. Being with.....
When you are with a person with dementia who is at end of life, you may not be communicating in a verbal manner. Non-verbal communication may be the focus as discussed in the previous pages. You have known and cared for your loved one – trust in your skills.
Research shows that attention to simple interventions makes a significant difference to how positively families viewed their relative’s death. ‘Being with’ rather than ‘doing for’ may be the aim or goal of care at this stage (Lawrence et al 2011).
9. Video Meeting Case Study
Tony, as you know, is 76 and has been living with Alzheimer's for approximately 9 years. Living at home with his wife Maura he needs 24 hour supervision. Tony worked as a shopkeeper and was always very diligent about record keeping and having all the household ‘bookwork in order’. He also loved spending time out in the garden.
Tony is back home from a two week Respite stay in a Nursing Home and is more confused than usual. Tony is rooting out all the letters in the house and moving them around. Maura finds this very frustrating.
Tony is also continually trying to get out to the garden, which is not safe for him to do alone as the steps are too steep and he had a fall there a few weeks ago. Maura is losing her patience and does not know how to solve these issues.
- What do we know of Tony that makes him a unique individual?
- What could Maura do to enhance Tony’s identity or personhood?
- How could Maura resolve the issues she is having with Tony within the home environment?
We will discuss these questions at the video workshop this week.